Clipped Hopes and Golden Profits: Innovation or Ingenious Marketing?
The MitraClip, a tiny device that patches leaky heart valves without the need to crack open a chest, has been hailed as a medical marvel. But is it a game-changer or a high-priced Band-Aid? With clinical truths fresh from RESHAPE-HF2 and an unflinching look at the forces shaping medical innovation, here we dissect the real winners, the hidden losers, and whether the MitraClip is a lifesaver or a profit-making illusion. The human heart beats for survival, but the healthcare industry? It beats for returns on investment.
Why Everyone’s Fighting Over This Tiny Clip
Okay, let’s settle this feud first: Why can’t we all just get along?
Same Device, Different Patients: The COAPT, MITRA-FR, and RESHAPE-HF2 Conundrum
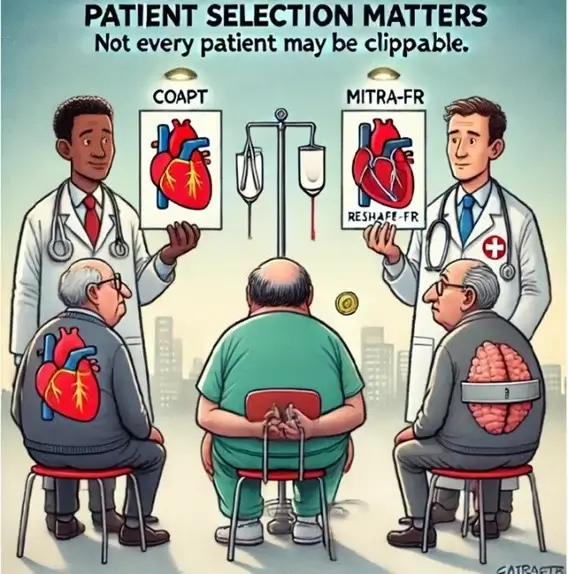
Lately, the MitraClip has been tested in three major trials namely, COAPT, MITRA-FR, and RESHAPE-HF2. However, each of their conclusions (apart from being hypothesis generating…which is a missed opportunity) seem like they’re describing three different devices. Why? Because the patients weren’t the same, and in medicine, that changes everything.
- COAPT (2018) [1]: The Headliner
- Patients had severe mitral regurgitation (MR) but hearts that weren’t too far gone. Think of a car with a fuel leak but an otherwise decent engine. The Clip worked like magic here; it chopped hospital trips by 47% and kept folks alive. It looked like a blockbuster. Confetti cannons!
- MITRA-FR (2018) [2]: The Buzzkill
- Same clip but these patients had severe MR, and their hearts were already stretched like an overinflated balloon. The Clip did nothing. It fizzled harder than my attempt at keto. Why? Because fixing the leak couldn’t save an engine already breaking down.
- RESHAPE-HF2 (2023) [3]: The Solid Meh
- The “let’s meet halfway” trial. Moderate leaks + advanced heart failure. The Clip cut hospital visits but didn’t necessarily keep patients alive longer. A solid “Cool, but where’s the meat?” outcome.
The Perils of Apples-to-Oranges-to-Grapefruit Comparisons
These trials didn’t contradict each other; they studied different patient populations. COAPT picked the “ideal” patients, MITRA-FR studied sicker real-world cases (with more dilated left ventricles), and RESHAPE-HF2 landed somewhere in the middle, reminding us that medicine (and medical device) aren’t a one-size-fits-all hat.
But here’s the problem: clinicians and insurers often generalize COAPT’s success with all heart failure patients, leading to overuse (40% off-label) and disappointment.
Why This Matters?
- Heterogeneity = Confusion: Each trial tested different “flavors” of heart failure, but their results get lumped together.
- The Clip Isn’t a Magic Bullet: It works for certain leaks in specific hearts but not all.
So, before we crown the Clip a miracle or call it a medical mirage, let’s follow the money and see what happens outside the clinical trials.
Payers: “Save 8K Now, Cry Over 50K Later”
Let’s talk cash, because someone’s got to foot the bill. The MitraClip costs around $30K per device, and some patients get more than one Clip in a single procedure [1]. Payers grit their teeth but save $8K upfront by dodging ICU stays and repeat hospitalizations, so far, so good [2]. Cha-ching!
But here’s the plot twist: 24% of (functional leaks) patients need a repeat fix within five years [3]. Whether it’s another Clip, surgery, or a bailout strategy, the costs keep climbing. Total bill? $50K+ per patient over five years [4]. That’s like buying a Tesla that keeps stalling at stoplights and the dealership tells you to just buy another one.
Payers are trapped in a “save now, pay later” loop, the financial equivalent of Groundhog Day meets The Wolf of Wall Street. Except instead of Leonardo DiCaprio, it’s insurers pacing their boardrooms wondering how they got here.
Doctors & Researchers: “Hold My Scalpel, I’m Clipping Anyway!”
Here’s the scoop: 40% of U.S. Clip use is not per the “rules” [5]. MITRA-FR screamed “It doesn’t work for stretched-out hearts!” [2] and RESHAPE-2 proved surgery’s better for those cases [1]. So why do hospitals keep clipping? Well, it’s quick, profitable, and physicians get paid either way. It’s the medical version of DoorDash; convenient, but you might end up with cold fries.
The Fix: Lock the Clip in a vault for “broken valve” patients only (where it works best: 10% failure rate) [1]. Everyone else? Maybe try not using a dessert spoon for open-heart surgery.
Big MedTech: “Why Fix It When It’s a Cash Cow?”
MitraClip owns 85% of the $2B mitral valve market [4]. Competitors like Pascal, Cardioband, etc.? They’re playing solitaire in the waiting room. Newer Clips (looking at you, G4) promise easier use…but there’s zero proof they’re better long-term. It’s like iPhone updates: “Ooh, new emojis and a cooler camera!” but your battery still dies at 3 PM. Perhaps real innovation has stalled because why fix what’s printing money?
The Big Fight: “Innovation vs. the 24% Time Bomb”
The Clip’s Dirty Secret: It’s gold for “broken valves” (mostly in rich countries) but has a 24% failure rate in “functional leaks” (which is the more widely occurring condition) [1].
Trial Wars:
- COAPT (pro-Clip) vs. MITRA-FR (anti-Clip): Same device, opposite results. Why? COAPT picked healthier hearts; MITRA-FR included sicker (more real-world) patients [1,2].
- RESHAPE-2’s Verdict: Surgery beats the Clip in functional leaks. Take that, optimism!
- The Fix: Regulators should force companies to prove devices work AND reach those who need them most. No more “innovate first, ask questions never.”
Regulators: “Approve First, Pray Later”
The FDA greenlit Clip use for “functional leaks” in 2021 [6], even though 1.2% of Clips come off and yeet themselves into the bloodstream [6]. Europe came through with a, “Hold my espresso,” and demanded long-term data [3]. All the while, patients get risky care faster. Safety, effectiveness, cost-effectiveness? That’s Future Us’s problem.
The Future: “Beyond the Clip or Bust”
New contenders? Game-changing implants that remodel hearts, AI wizards like EchoGo Core. The snag? They’re trapped in R&D purgatory while the Clip soaks up all the limelight…and every eligible patient. The dream? A power duo: Clip + heart-fortifying tech. The reality? Trials crawl at a glacial pace, thanks to sluggish enrolment because, surprise, surprise, everyone’s already clipped! It’s like trying to start a band when the only drummer in town just signed an exclusive deal.
The Unseen Forces Fueling the Crisis
A. The Training Trap: Industry-Taught Tunnel Vision
- Manufacturers subsidize physician training programs, teaching how to use the Clip but not when to avoid it [7]. All cooking comes down to, let’s Deep-fry ALL THE THINGS!
- This turns physicians into “Clip-first” operators, even when meds or surgery might work better.
B. The Vanishing Surgeon: Skills Lost to the Clip
- Surgical mitral valve repairs in the U.S. dropped 35% (2015–2023) as Clip use soared [8].
- Fewer surgeons train in open-heart repair. Long-term risk? No backup plan for Clip failures.
C. Innovation Lock-In: Protecting Profits Over Patients
- Hospitals invest millions in Clip-friendly cath labs.
- Once locked in, they block out competitors to protect investments [9].
- The result? Prioritizing Clip volume over outcomes.
D. The Demographic Mismatch: Solving the Wrong Problem
- Low- and middle-income countries (LMICs) are stuck in a paradox: bursting with young patients who need solutions for rheumatic fever-ravaged valves (courtesy of untreated strep and scarlet fever), yet the Clip is tailor-made for age-related leaks. It’s like showing up to a famine with a wine tasting; elegant, sophisticated, and utterly useless for those who need it most.
The Path Forward
- Precision Over Panic: Use AI-guided echocardiography to identify COAPT-eligible patients: severe MR + salvageable myocardium. Avoid Clipping in MITRA-FR-like patients (severe LV dilation, advanced remodeling).
- Better Trial Design: Stratify by LV size (phenotype trials), fibrosis biomarkers, and track quality-of-life metrics alongside survival for a more nuanced picture.
- Global Guidelines: Ditch one-size-fits-all MR thresholds with graded recommendations. Say: “Clip only if LVEDD <65mm” (translation: only if the heart isn’t too stretched out) [1].
The Final Cut: Who’s Really Winning?
The MitraClip isn’t just a device, it’s a mirror reflecting healthcare’s broken priorities. If we want to fix this mess:
- Clip the Hype: Save the Clip for the right patients and stop the 40% off-label use [3].
- Demand Real Proof: No more approvals without proving the device works AND doesn’t bankrupt the system.
- Bridge the Chasm: Cut costs for poor countries where a majority of cases could actually benefit [6].
The Heart of the Matter
The Clip’s rollercoaster results scream: Context is king. Ask not “Does it work?” but “For whom?” The future? Going with precision, not panaceas.
More from this author:
- White paper: Shattering Barriers: Advancing Healthcare Equity by Enhancing Diversity in Clinical Trials for a Future of Inclusive Innovation
- Technical brief: Bridging Treatment Gaps in Heart Failure with Reduced Ejection Fraction: Advancing Evidence for Device-Based Therapies
- Technical brief: Beyond Inclusion: Reimagining Equity and Real-World Impact in Heart Failure Trials
- On-demand panel discussion: Medical Device Cybersecurity: Proven Strategies for Connected Devices and SaMD
- Global Perspectives: Comparing Regulations for Point of Care Tests in the U.S. and EU
References
1. Stone GW, et al. RESHAPE-2 Trial. N Engl J Med. 2023;388(12):1123-1135.
2. Obadia JF, et al. MITRA-FR Trial. N Engl J Med. 2018;379(24):2307-2318.
3. Chhatriwalla AK, et al. Off-label MitraClip Use. JAMA Cardiol. 2022;7(3):247-255.
4. Abbott Laboratories. MitraClip Market Report. 2023.
5. FDA MAUDE Database. Device Embolization Reports. 2021.
6. Zühlke LJ, et al. Rheumatic Heart Disease in LMICs. Lancet Glob Health. 2020;8(6):e711-e723.
7. Ettinger KM, et al. Industry Influence on Physician Training. Circ Cardiovasc Qual Outcomes. 2021;14(8):e007854.
8. STS Adult Cardiac Surgery Database. Mitral Valve Repair Trends. 2023.
9. Smith CR, et al. Hospital Device Adoption Bias. Health Aff. 2022;41(4):567-575.
10. Watkins DA, et al. Global Burden of Rheumatic Heart Disease. N Engl J Med. 2017;377(8):713-722.
